Cognition: Pieces of the Puzzle
Cognitive symptoms are a near-ubiquitous core feature of schizophrenia,1,2 impacting at least 80% of patients with schizophrenia, with varying degrees of severity.3,4 Cognitive symptoms are associated with reduced medication adherence, reduced employment rates, the inability to live independently, interpersonal difficulties, and a reduced quality of life.5–7 Cognitive impairment is not a unitary concept but rather is a set of impairments to the constituent cognitive domains; typically patients with schizophrenia perform at approximately one standard deviation below the level of healthy individuals in any given cognitive domain.5 Despite the high prevalence of cognitive symptoms and the debilitating effects they have on daily life,1–8 there are no approved pharmacotherapies targeting these symptoms, and access to behavioral treatments (e.g. cognitive remediation therapy) can be limited by factors such as geographic location.9,10
Impairments across cognitive domains in schizophrenia
We commonly refer to seven cognitive domains: speed of processing, attention/vigilance, social cognition, working memory, verbal learning, visual learning, and reasoning/problem solving.11–13 These distinctions are supported by the conclusions of the Neurocognition Committee of the Measurement and Treatment Research to Improve Cognition in Schizophrenia (MATRICS™).11–13 Formal assessments of each domain are included in the MATRICS Consensus Cognitive Battery (MCCB™) which consist of 10 tests.11–13 Beyond formal assessments, it is crucial to understand that these impairments can manifest in a variety of ways,5 and multiple impaired domains can significantly impact patients’ daily lives.14
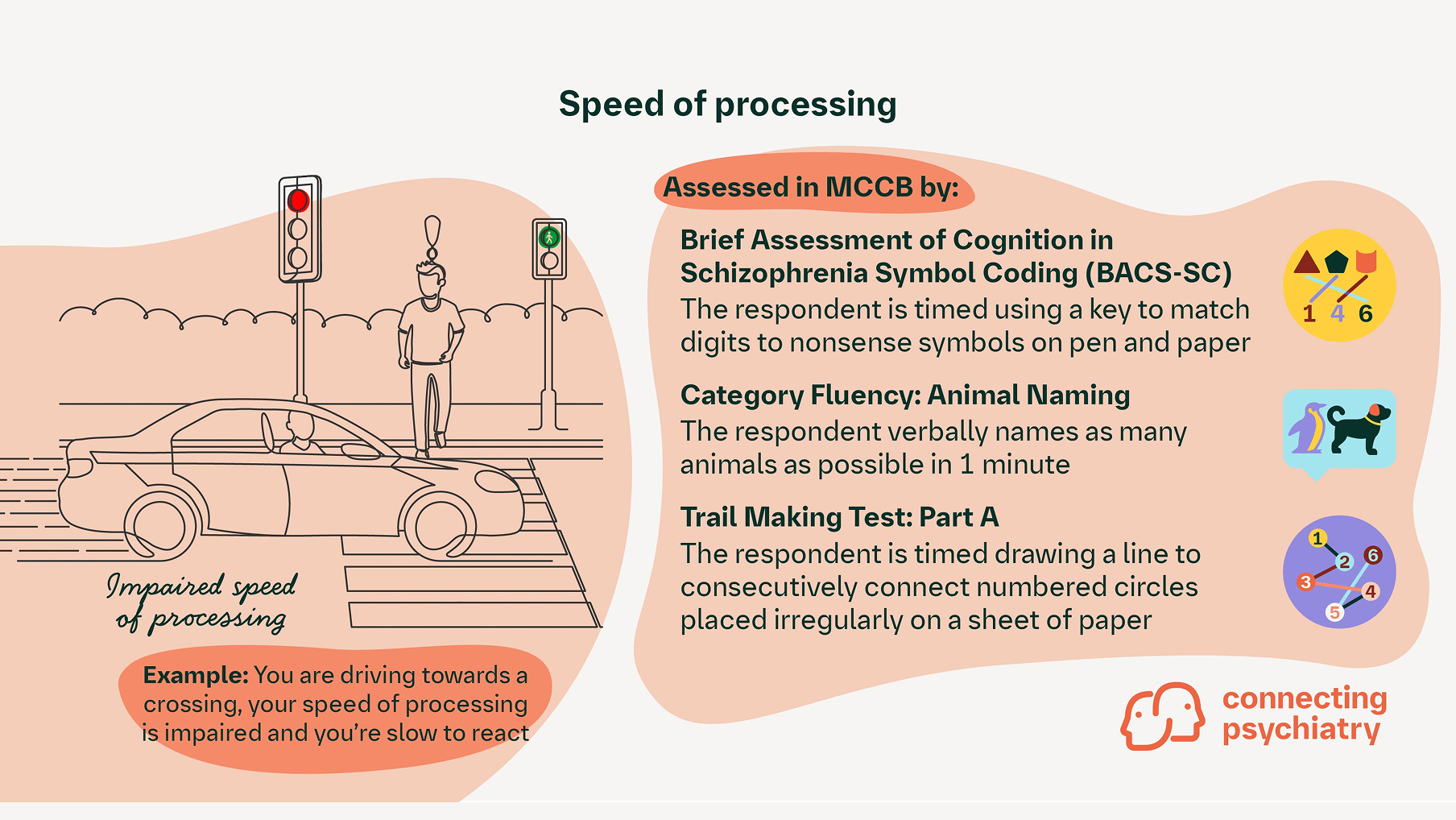
Speed of processing:
Pertains to an individual’s ability to respond quickly and accurately when performing perceptual, motor, or cognitive tasks15
Impaired processing speed is an important predictor of functional outcome in patients, and it may predict conversion to a full-blown psychotic disorder in at-risk patients16
Example: Imagine that you are paying for something with some change, your speed of processing is impaired, and you struggle to count out the correct coins
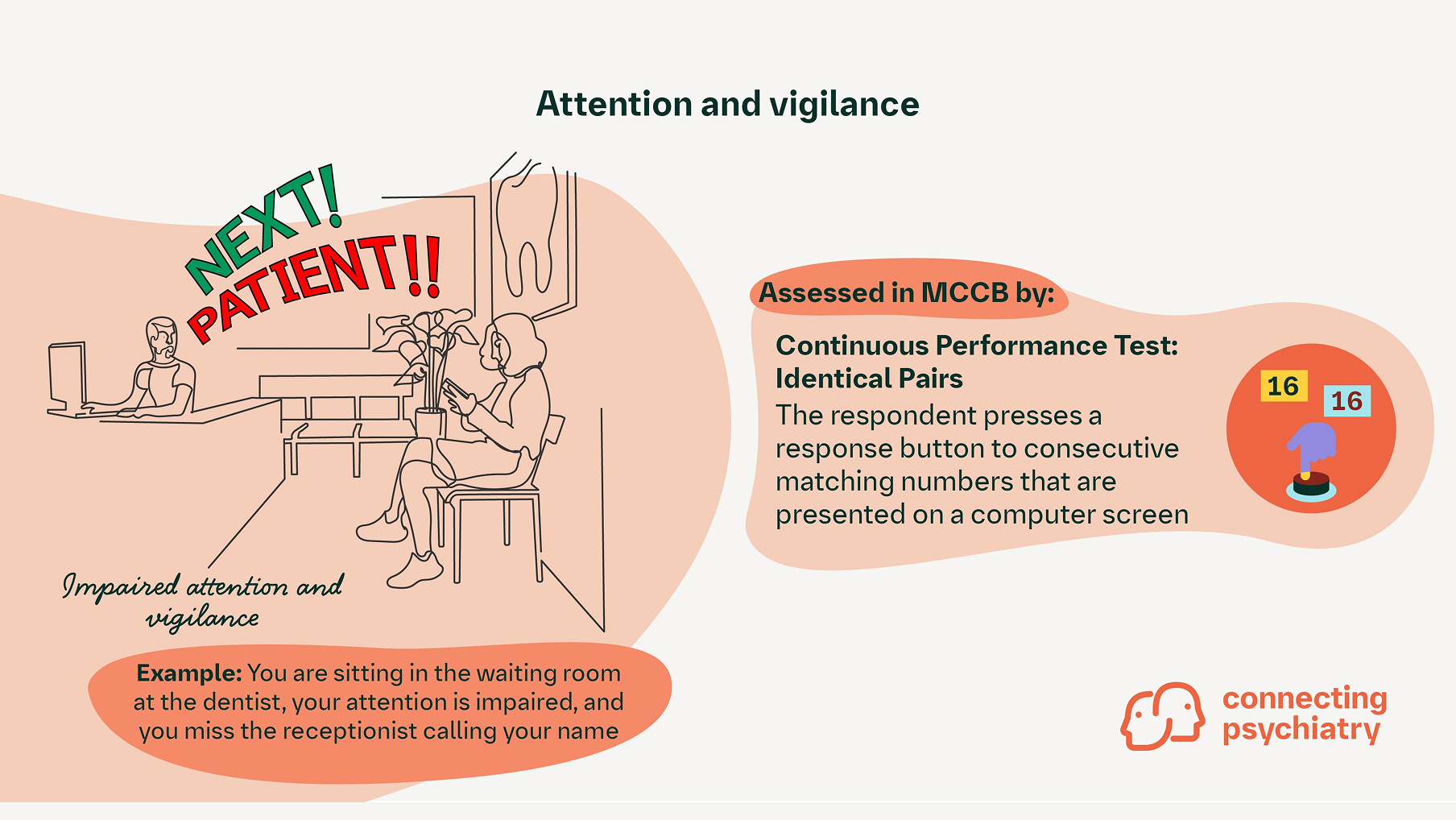
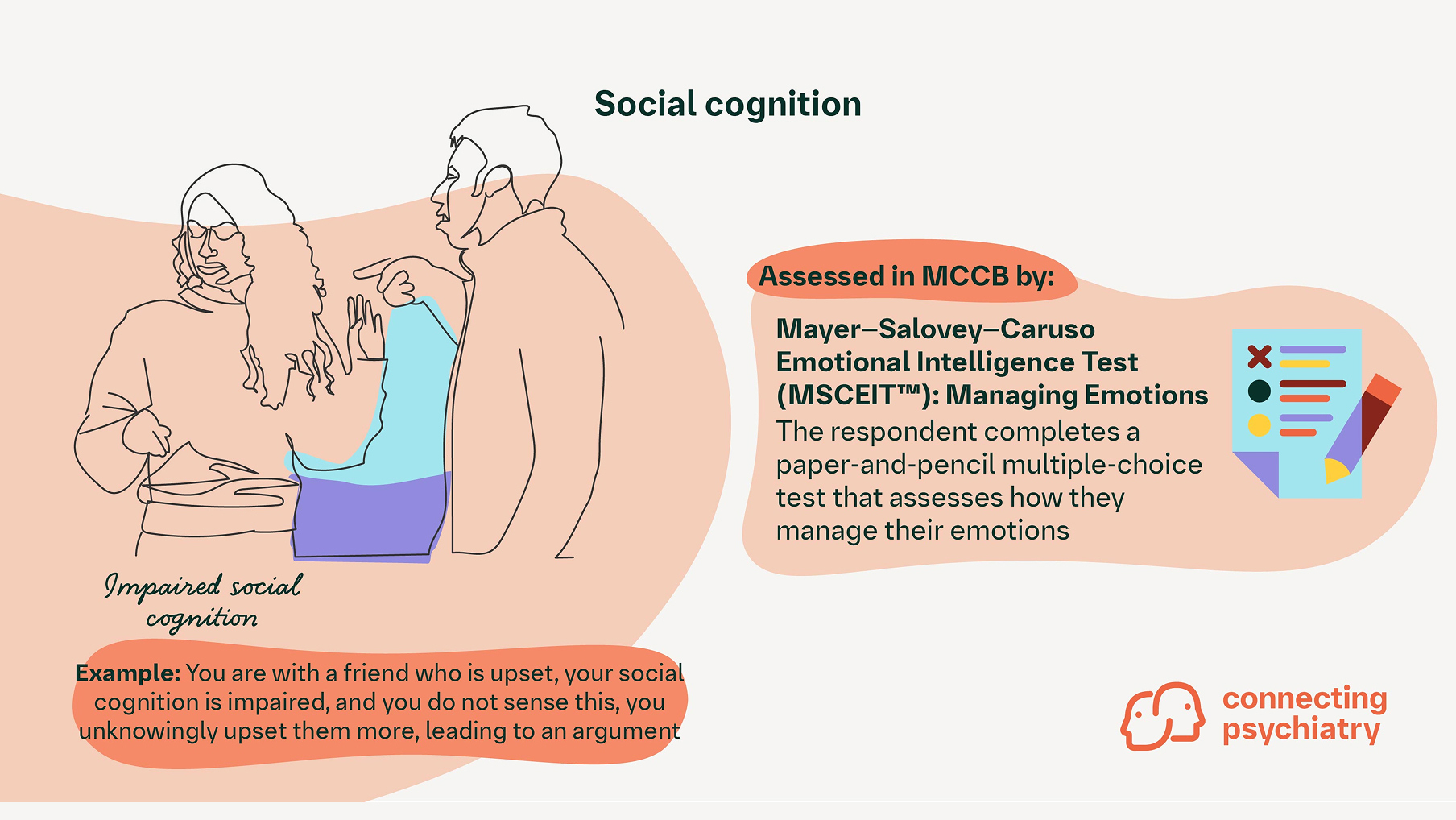
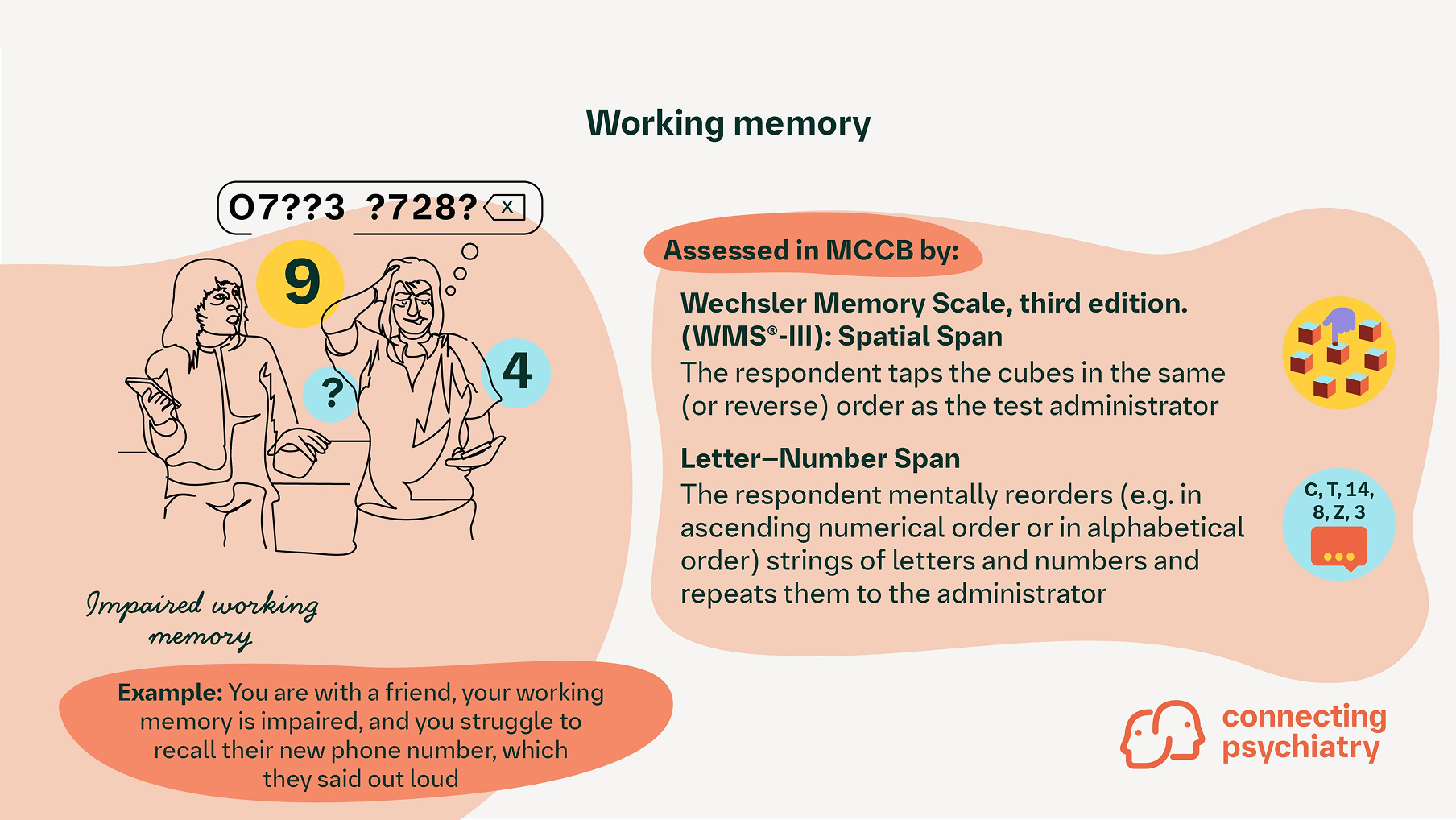
For each domain, the figure shows another example of real world impact, as well as the test(s) used to formally assess performance and identify impairment
Attention/vigilance:
Pertains to the awareness of and attendance to a stimulus or set of stimuli. Vigilance is the capacity to maintain attention over an extended period of time17
Impairments in attention/vigilance is one of the earliest cognitive symptoms associated with schizophrenia to manifest in patients18
Real world example: Imagine you are sitting in a university lecture, your attention is impaired, and you miss the lecturer asking you a question
Social cognition:
Refers to the interpretation of information about others such as their character, intentions, and behaviour17
Social cognition represents a domain in which impairments can result in social isolation, exacerbation of symptoms, and the promotion of relapses18,19
Real world example: Imagine you invite your friends for a get-together, but they are busy, your social cognition is impaired, and you interpret this as they do not want to spend time with you
Working memory:
Involves the evaluation, manipulation, and synthesis of newly acquired information17
Impairments in working memory can make it difficult for patients to handle social and interpersonal situations that require attention to multiple streams of information20
Real world example: Imagine you are with your friends at a restaurant and you’re placing the order, your working memory is impaired, and you struggle to recall everyone’s orders
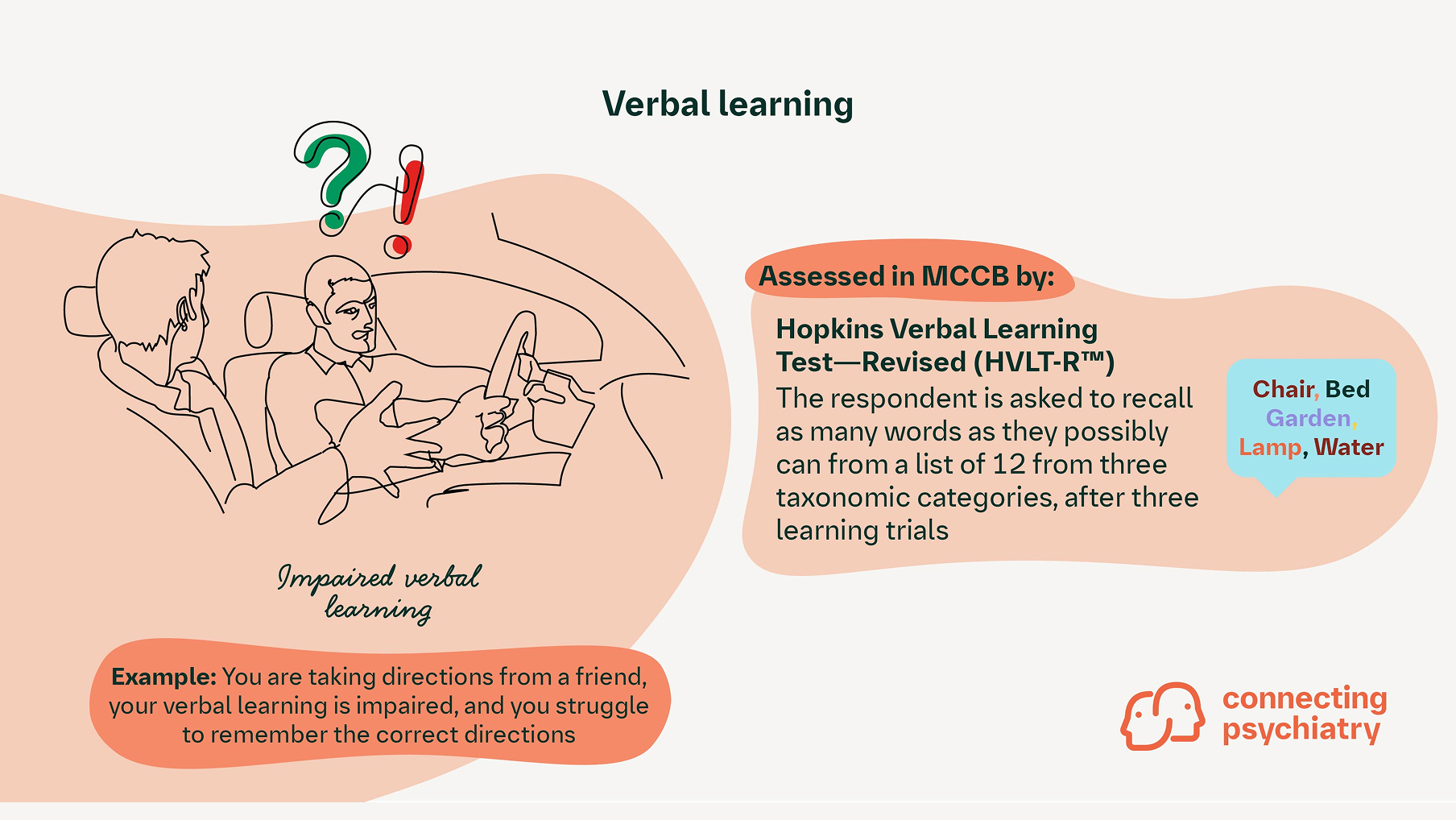
Verbal learning:
Refers to the ability to recall previously spoken information21
Strongly associated with measures of functional outcome in addition to community outcome, and the acquisition of new skills22
Real world example: Imagine your sibling is telling you what to buy from the supermarket, your verbal learning is impaired, and you struggle to remember the items
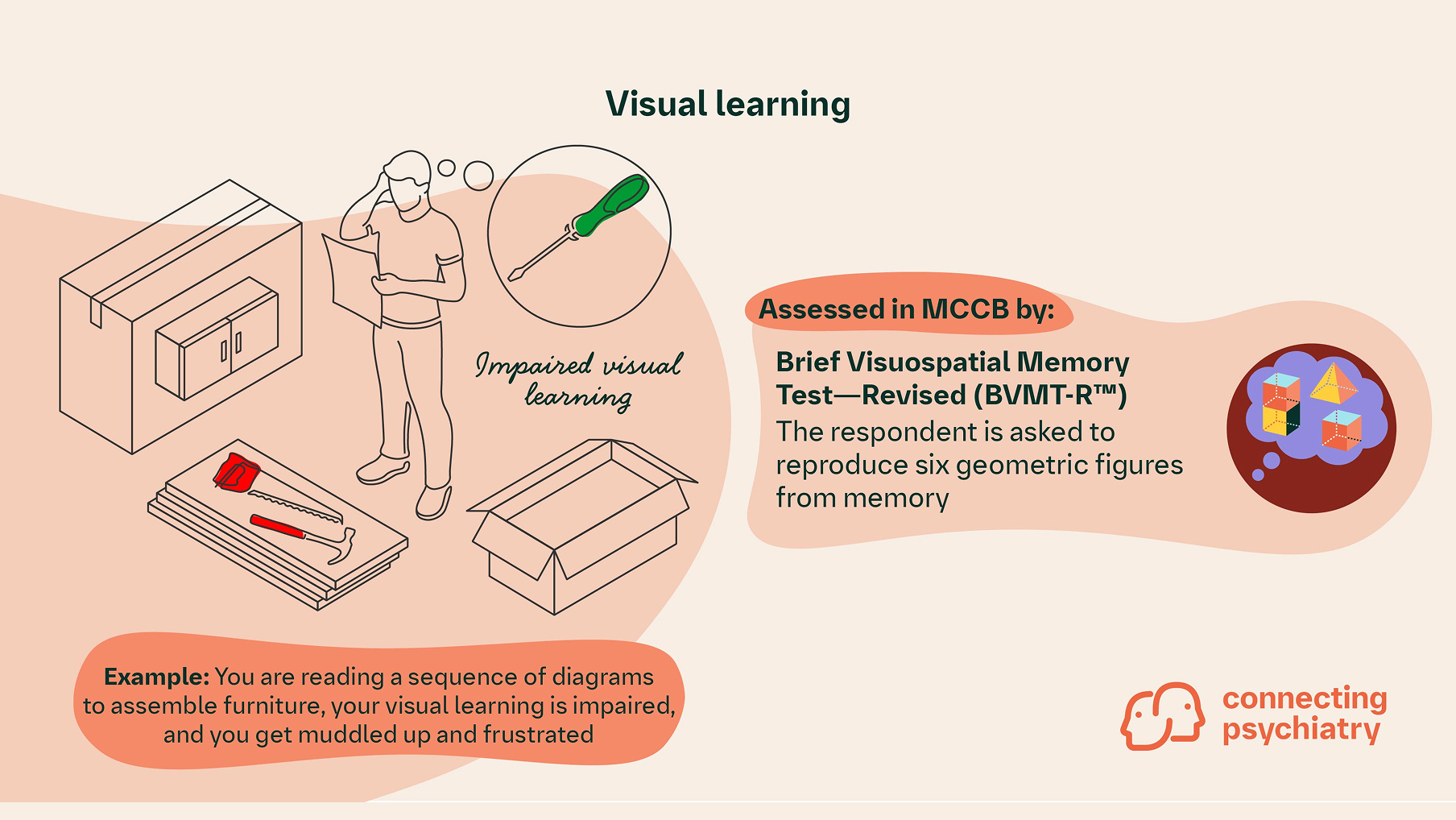
Visual learning:
Refers to the ability acquire, store, and retrieve information about objects and spatial locations15
Impairment in visual memory and visual motor speed may be evident before the onset of psychotic symptoms,18 which is an important note for physicians and healthcare professionals
Real world example: Imagine you are studying a floor plan, your visual learning is impaired, and you struggle to find the right room for a medical appointment
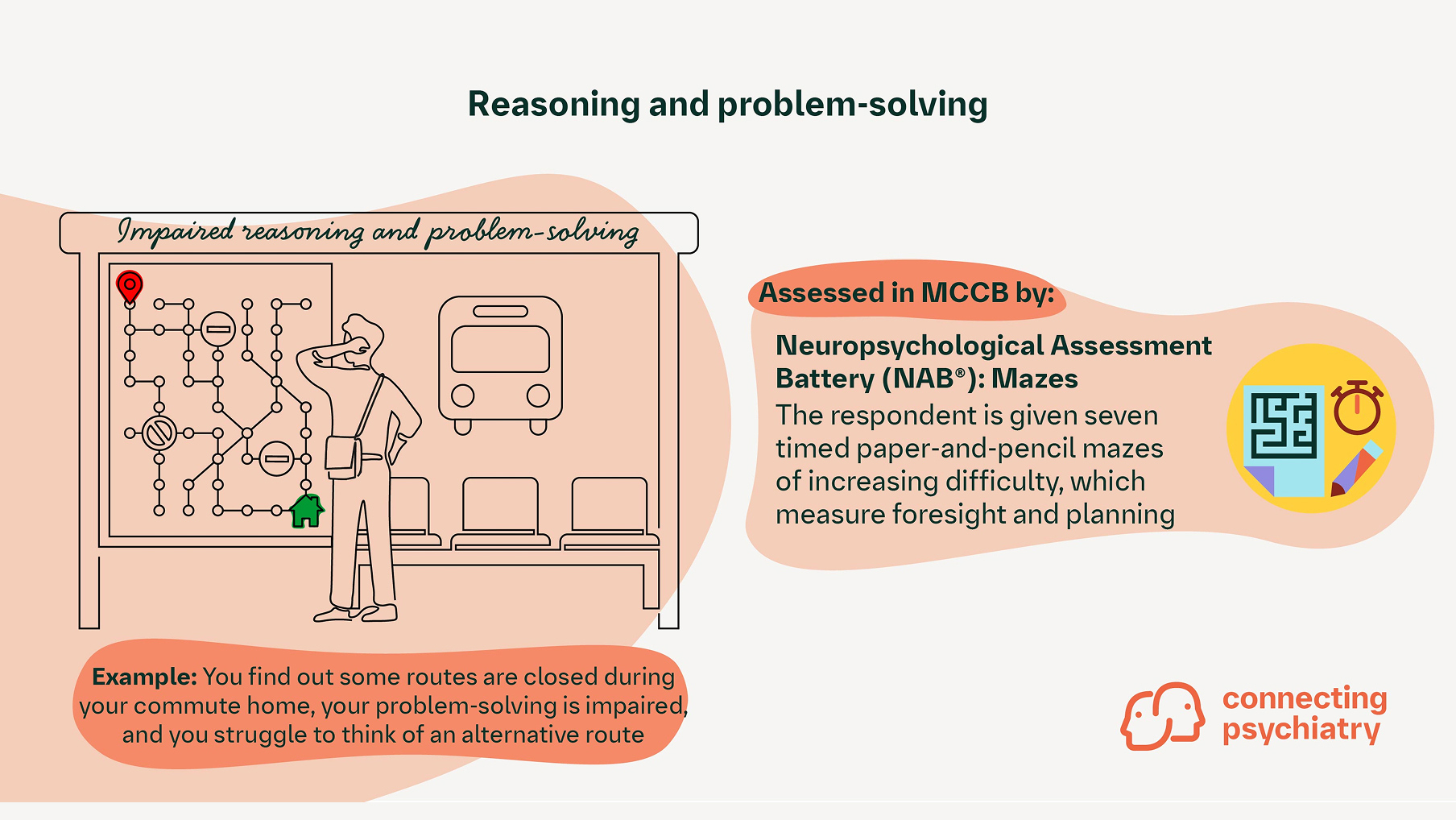
Reasoning/problem-solving:
Refers to the ability to apply and shift strategies effectively to find optimal solutions15
Impaired reasoning and problem-solving skills in patients with schizophrenia can affect their ability to live independently, contribute to disability, and be the cause of incautious and hasty decision-making23,24
Real world example: Imagine there is a festival in town, your reasoning is impaired, and you don’t infer that traffic is likely to be worse than normal, making you late to your appointment
Bringing it back to the clinic
Clinicians may find that the way impairments in cognitive domains translate to real-life impact differs widely between patients. Consider if any of the examples above resonate with discussions you may have had with your own patients. It is important to acknowledge that the MCCB takes some time to administer and in clinical practice, it may be more suitable to use another tool. Despite development of assessment tools for use in the clinic, concerns around coverage of domains or duration and ease of implementation mean there is limited uptake.5,25 Beyond formal assessment, in clinical practice one option is an open discussion focusing on patients' experiences, challenges and goals.
Cite this article as Cognition: Pieces of the Puzzle. Connecting Psychiatry. Published May 2024. Accessed [month day, year]. [URL]
BACS SC, Brief Assessment of Cognition in Schizophrenia Symbol Coding; BVMT-R, Brief Visuospatial Memory Test—Revised; HVLT-R, Hopkins Verbal Learning Test—Revised; MATRICS, Measurement and Treatment Research to Improve Cognition in Schizophrenia; MCCB, MATRICS Consensus Cognitive Battery; MSCEIT, Mayer–Salovey–Caruso Emotional Intelligence Test; NAB, Neuropsychological Assessment Battery; WMS-III, Wechsler Memory Scale, third edition.
-
Bora E, et al. Schizophr Bull 2010;36:36–42.
-
Harvey PD, et al. Schizophr Res Cogn 2022; doi: 10.1016/j.scog.2022.100249.
-
Mosiołek A, et al. BMC Psychiatry 2016;16:37.
-
Keefe RSE, et al. Biol Psychiatry 2005;57:688–691.
-
McCutcheon RA, et al. Mol Psychiatry 2023; doi: 10.1038/s41380-023-01949-9.
-
Tripathi A, et al. Clin Psychopharmacol Neurosci 2018;16:7–17.
-
Kitchen H, et al. Adv Ther 2012;29:148–162.
-
Iasevoli F, et al. Psychiatry Res 2017;249:159–166.
-
Keefe RSE. World Psychiatry 2019;18:167–168.
-
Altman RAE, et al. Can J Psychiatry 2023;68:139–151.
-
MATRICS. List of Tests. 2023. Available at: https://www.matricsinc.org/mccbtestlist/. Last accessed: May 2024.
-
Nuechterlein KH, et al. Am J Psychiatry 2008;165:203–213.
-
Keefe RSE, et al. Schizophr Res 2011;125:161–168.
-
Harvey PD, et al. Schizophr Res 2012;140:1–8.
-
Green MF, et al. World Psychiatry 2019;18:146–161.
-
Karbasforoushan H, et al. Psychol Med 2015;45:109–120.
-
Millan MJ, et al. Nat Rev Drug Discov 2012;11:141–168.
-
Mihaljević-Peleš A, et al. Psychiatr Danub 2019;31:139–142.
-
Fett A-KJ, et al. Neurosci Biobehav Rev 2011;35:573–588.
-
Bowie CR & Harvey PD. Neuropsychiatr Dis Treat 2006;2:531–536.
-
Holmlund TB, et al. NPJ Digit Med 2020; doi: 10.1038/s41746-020-0241-7.
-
Schulz CS & Murray A. J Clin Psychiatry 2016;77:3–7.
-
Moritz S, et al. Schizophr Bull 2006;32:327–331.
-
Xia J & Li C. Cochrane Database Syst Rev 2007;2007:CD006365.
-
Keefe RSE, et al. Schizophr Res 2004;68:283–297.
SC-US-77042
SC-CRP-16152
July 2024
Related content
Schizophrenia Primer 3 of 3: Cognitive Impairment Associated With Schizophrenia (CIAS)
Sign up now for new features
The newsletter feature is currently available only to users in the United States
*Required field

