Article in Focus
A Renewed Focus on Negative Symptoms of Schizophrenia?
A new era for the negative symptoms of schizophrenia.
– Fernandez-Egea E, et al. Br J Psychiatry 2023;223:269–2701

A major unmet need
In a recent review, Fernandez-Egea and colleagues reviewed the current state of the art for the management of negative symptoms for people with schizophrenia. The authors concluded that negative symptoms represent a major unmet need, with treatment options such as antipsychotics focused on the management of positive symptoms. While antipsychotics have shown some efficacy in treating these positive symptoms, the quality of life for many patients is still affected by negative and cognitive symptoms, representing a clear unmet treatment need.
How can the field progress?
Combining a transdiagnostic approach using the National Institute of Mental Health’s Research Domain Criteria framework with a computational approach may help to elucidate the various components of negative symptoms from patient to patient. Rating scales such as the Scale for the Assessment of Negative Symptoms, or SANS, and the Positive and Negative Syndrome Scale, or PANSS, remain important for the definition and assessment of negative symptoms. Second-generation scales were developed to be more comprehensive, assessing not only the observed behavior but also internal experiences. One such tool is the Clinical Assessment Interview for Negative Symptoms, or CAINS. Ultimately, future studies should leverage these tools and recruit populations that are more representative of the heterogeneous nature of schizophrenia to allow robust conclusions to be drawn.
Different neuropathophysiologies may underlie each negative symptom domain
“Negative symptoms of schizophrenia” is an umbrella term with at least two distinct dimensions:1,2
Experiential, which includes: | Expressive, which includes: |
The authors concluded that there is growing evidence to suggest that each of the five domains may have different underlying biological mechanisms:
- The expressive dimension, not the experiential dimension, correlates with the thinning of specific frontal lobe areas in a cohort of patients with first-episode psychosis over a 10-year follow-up period3
- Clozapine-induced sedation negatively impacts the experiential dimension of the Brief Negative Symptom Scale (BNSS) but not the expressive dimension4
- Abnormal perception of stress in patients reporting early-age abuse is a potential risk factor for anhedonia, independent of the disorder, which may suggest that adverse childhood events are a risk factor for negative symptoms5
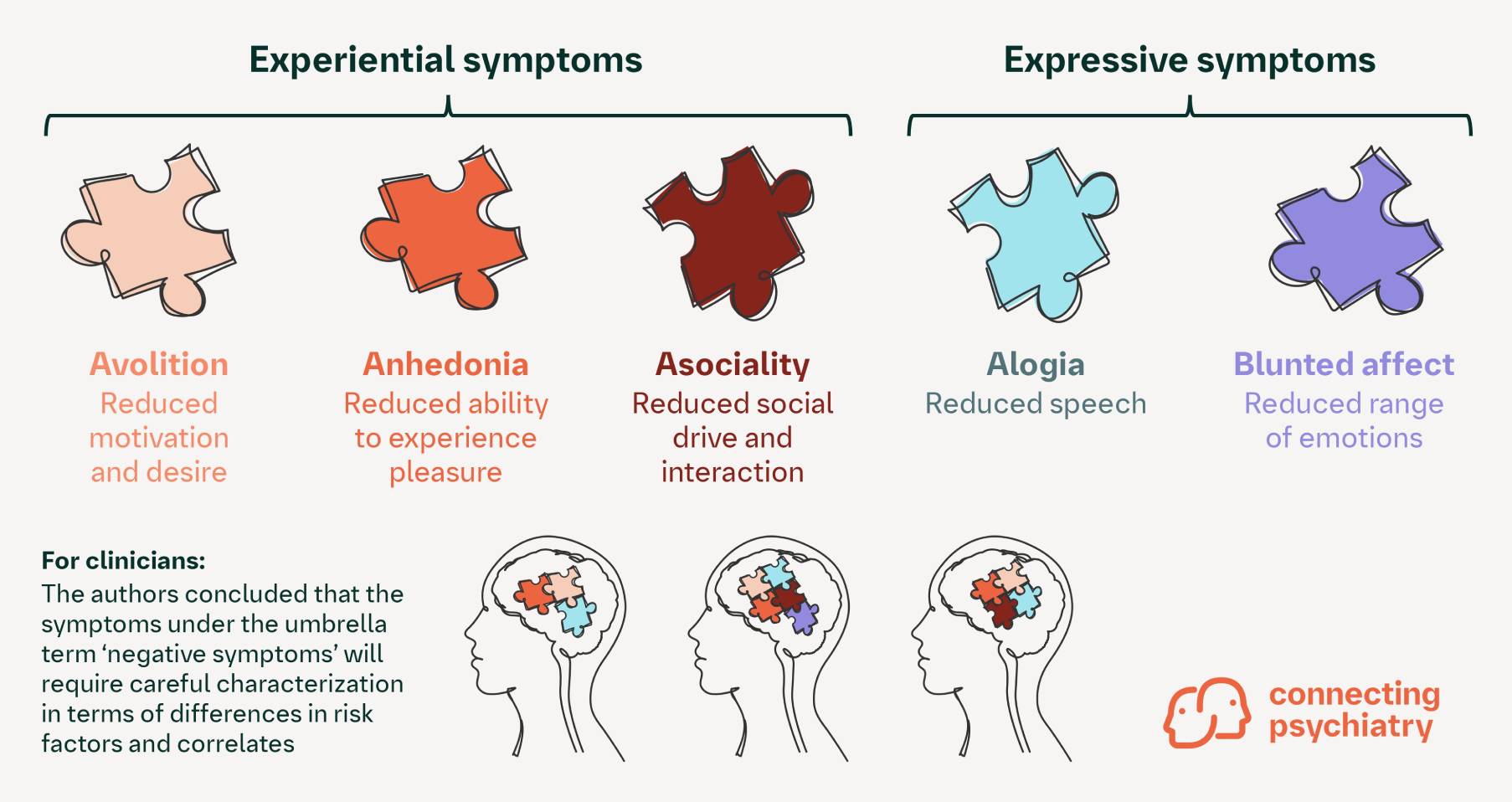
The authors concluded that:
- Poor characterization of negative symptom domains is a major obstacle to the development of treatments that are suited to each individual
- Careful characterization of negative symptoms will become increasingly important as more evidence emerges about the differences among the five domains of negative symptoms
- Refinement in the assessment and neuroscience modeling of negative symptoms has the potential to lead to a new era of clinical epidemiology, pathophysiological studies, and treatment trials
Cite this article as Article in Focus. Connecting Psychiatry. Published April 2025. Accessed [month day, year]. [URL]
BNSS, Brief Negative Symptom Scale; CAINS, Clinical Assessment Interview for Negative Symptoms; PANSS, Positive and Negative Syndrome Scale; SANS, Scale for the Assessment of Negative Symptoms.
-
Fernandez-Egea, et al. Br J Psychiatry 2023;223:269–270.
-
Stahl SM. Stahl’s Essential Psychopharmacology, 5th ed., 2021. Cambridge University Press.
-
Canal-Rivero M, et al. Br J Psychiatry 2023;223:309–318.
-
Wolpe N, et al. Br J Psychiatry 2023;223:295–297.
-
O'Brien KJ, et al. Br J Psychiatry 2023;223:273–279.
SC-US-76942
SC-CRP-16117
March 2024
Related content

More Than the Sum of Its Parts: The Etiology of Schizophrenia
Sign up now for new features
The newsletter feature is currently available only to users in the United States
*Required field