Article in Focus
Does Cognitive Function Moderate the Association Between Inner Speech and Hallucinations in Schizophrenia?
The moderating effect of cognitive impairment on the relationship between inner speech and auditory verbal hallucinations among chronic patients with schizophrenia
– Mahfoud D, et al. BMC Psychiatry 2023;23:431.1

ASSOCIATION BETWEEN COGNITIVE IMPAIRMENT AND AUDITORY VERBAL HALLUCINATIONS
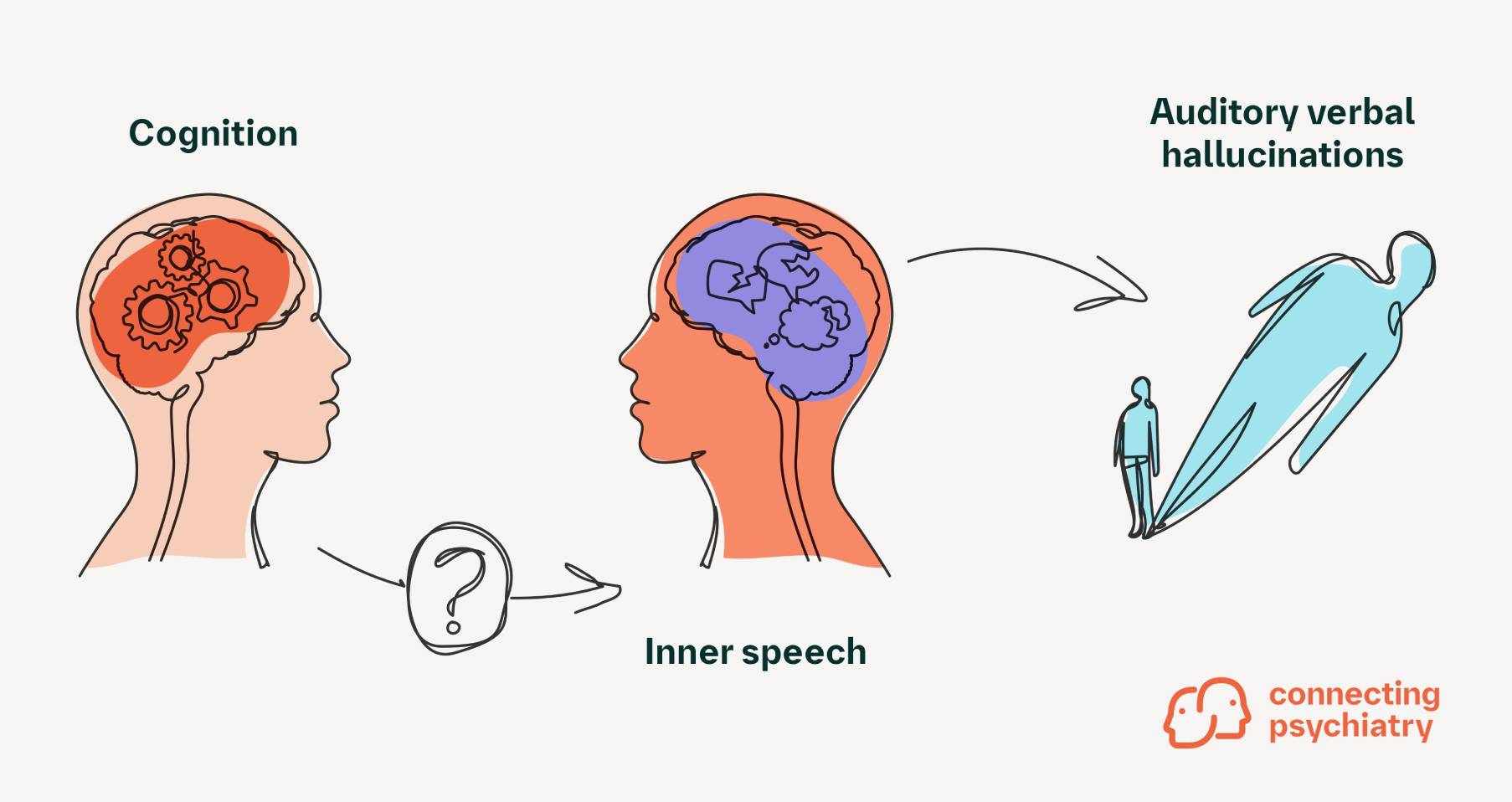
Auditory verbal hallucinations (AVH) are the most common type of hallucination in patients with schizophrenia and affect nearly two-thirds of patients. These hallucinations include subjective perceptual experiences of voices, typically other than self, that occur while the patient is fully conscious; there are no external stimuli present during these episodes.1,2 Abnormalities in inner speech, the self-centric voice in our heads that narrates our daily lives, may underlie some aspects of AVH. However, further research to investigate the relationship between inner speech and AVH is needed.1,2
Although the precise relationship between inner speech and AVH is not fully understood, several symptom moderators that may affect this association have been identified. One such factor is cognitive impairment, which occurs in 70%–80% of patients with schizophrenia.1
Cognitive impairment has previously been linked to uncontrolled inner speech that can result in inner speech–based AVH.3 To better understand this relationship, Mahfoud et al evaluated whether degree of cognitive function (low, moderate, and high) is correlated with inner speech and subsequent AVH in Lebanese patients with schizophrenia.1

This cross-sectional study was conducted between May and August of 2022 at the Psychiatric Hospital of the Cross in Lebanon and included randomly selected inpatients aged 18 years or older with chronic schizophrenia per Diagnostic and Statistical Manual of Mental Disorders, 5th Edition criteria. To participate in the study, patients must have had the cognitive ability to fill out a questionnaire. All data were gathered in face-to-face structured interviews with each participant.
Each patient completed three different questionnaires to assess varying aspects of cognition, inner speech, and AVH:
- Montreal Cognitive Assessment (MoCA) Test: detects mild cognitive impairment
- Varieties of Inner Speech Questionnaire – Revised (VISQ-R): assesses characteristics of inner speech across multiple subscales
- Psychotic Symptom Rating Scales (PSYRATS): evaluates the severity of delusions and auditory hallucinations
Of the 207 patients recruited for the study, 189 were included in the evaluation. The mean age of patients was 57.3 years (SD, 11.2 years) and the majority of patients were male. Most patients were of a low socioeconomic status and many were illiterate.
Patients who perceived inner speech as originating from an external entity had higher scores on the other people in inner speech subscale of the Varieties of Inner Speech Questionnaire – Revised assessment; they also experienced significantly more hallucinations than those with lower scores
(β= 0.96; t=4.454; p<0.001). Interestingly, cognitive function was not associated with hallucinations (β=0.25; t=0.993; p=0.322).
However, after controlling for delusions and adjusting for other factors, such as level of education, socioeconomic status, and age, the interaction between cognitive performance and score on the other people in inner speech subscale was significantly associated with hallucinations (p<0.01). Low (β=0.69; t=5.048; p<0.001) or moderate (β=0.45; t=4.096; p<0.001) cognitive performance and the presence of other people in inner speech subscale were significantly associated with increased occurrence of hallucinations. Other people in inner speech was not associated with hallucinations in patients with high cognitive performance.
Although this study showed evidence for cognitive impairment as a potential moderator of the relationship between inner speech and AVH, the neurobiological mechanisms that underlie this interaction require further investigation. Employing other methods that do not rely on self-reporting, such as experience sampling, may help parse out the moderating effect of cognition on inner speech and AVH in greater detail.
ADDRESSING UNDERLYING COGNITIVE SYMPTOMS COULD IMPROVE AVH
An improved understanding of the relationship between inner speech and the onset of AVH is needed. Deciphering whether cognitive impairment impacts the relationship between inner speech and AVH could help establish novel management plans, including pharmacological and behavioral interventions, that can reduce the burden of hallucinations for these patients.
Despite the findings of this study, additional longitudinal studies will be needed to fully understand the moderative effects of cognition on inner speech and AVH. Further, it is important to note that the relationship between cognitive functioning and inner speech is complex, and findings may vary depending on the specific cognitive task used or cognitive domains assessed. Regardless, the high incidence of cognitive impairment in schizophrenia necessitates further research on how cognition impacts inner speech and AVH; such research could lead to improvements in the lives of many patients living with schizophrenia.
- It has been shown that cognitive function has a moderating effect on the relationship between inner speech and AVH, after controlling for delusions; this effect is dependent on the patient’s level of cognitive function
- Cognitive impairment may contribute to a deficit in monitoring of inner speech, which may then lead to voices of others in inner speech being misattributed to external voices
Cite this article as Article in Focus. Connecting Psychiatry. Published April 2025. Accessed [month day, year]. [URL].
-
Mahfoud D, et al. BMC Psychiatry 2023;23:431.
-
De Leede-Smith S & Barkus M. Front Hum Neurosci 2013;7:367.
-
Brébion G, et al. Front Psychol 2016;7:1381.
SC-CRP-15441
SC-US-76912
March 2024
Related content

More Than the Sum of Its Parts: The Etiology of Schizophrenia
Sign up now for new features
The newsletter feature is currently available only to users in the United States
*Required field

