Factor It In: A New Movement for Mental Health
The Factor It In series will illuminate the influences on mental health that arguably deserve greater attention. You will be provided with fresh perspectives through a discussion of the factors that impact the development of serious mental health conditions and a review of the literature on impact on disease course; ultimately, you may use this knowledge to inform discussions with your patient.
In summary
|
The Greek physician Hippocrates was the first medical figure on record to provide a written prescription for exercise for the treatment of a health condition, famously stating that “walking is a man’s best medicine.”8,9 In an increasingly sedentary world, the benefits of regular exercise cannot be overstated. While modern medicine has revolutionized the treatment of nearly all health conditions, incorporating physical activity and exercise into our routines can have therapeutic benefits to many aspects of our lives, such as managing body weight, boosting energy, and improving mental health.10,11 In fact, the European Psychiatric Association, the German Association for Psychiatry, Psychotherapy and Psychosomatics, and the American Psychiatric Association all promote exercise as beneficial to mental health, and recommend incorporating exercise routines into treatment plans for individuals with mental health disorders.12–14 In this article, we explore how exercise impacts brain physiology, alleviates symptom burden, and improves quality of life in these individuals.
Distinguishing between physical activity and exercise
Though physical activity and exercise are often used interchangeably, each term describes distinct concepts that are essential to their application in medicine.15 The medical community defines physical activity as any bodily movement produced by skeletal muscle that results in energy expenditure, whereas exercise comprises a subset of physical activity that is planned, structured, and repetitive, with a focus on maintaining physical fitness.9 Exercise can take many forms, from cycling or lifting weights to a weekly game of football at the pitch with friends.
The impact of exercise on brain chemistry and structure
Neuroimaging studies have shown abnormal patterns of activity in brain regions such as the hippocampus, amygdala, and some regions of the cerebral cortex, in patients with mental health conditions compared with healthy individuals.16 At a neural circuit level, mental health disorders may disrupt fundamental aspects of neural plasticity, which, in turn, negatively impact the flow and processing of information in the brain, giving rise to neurobehavioral symptoms.1
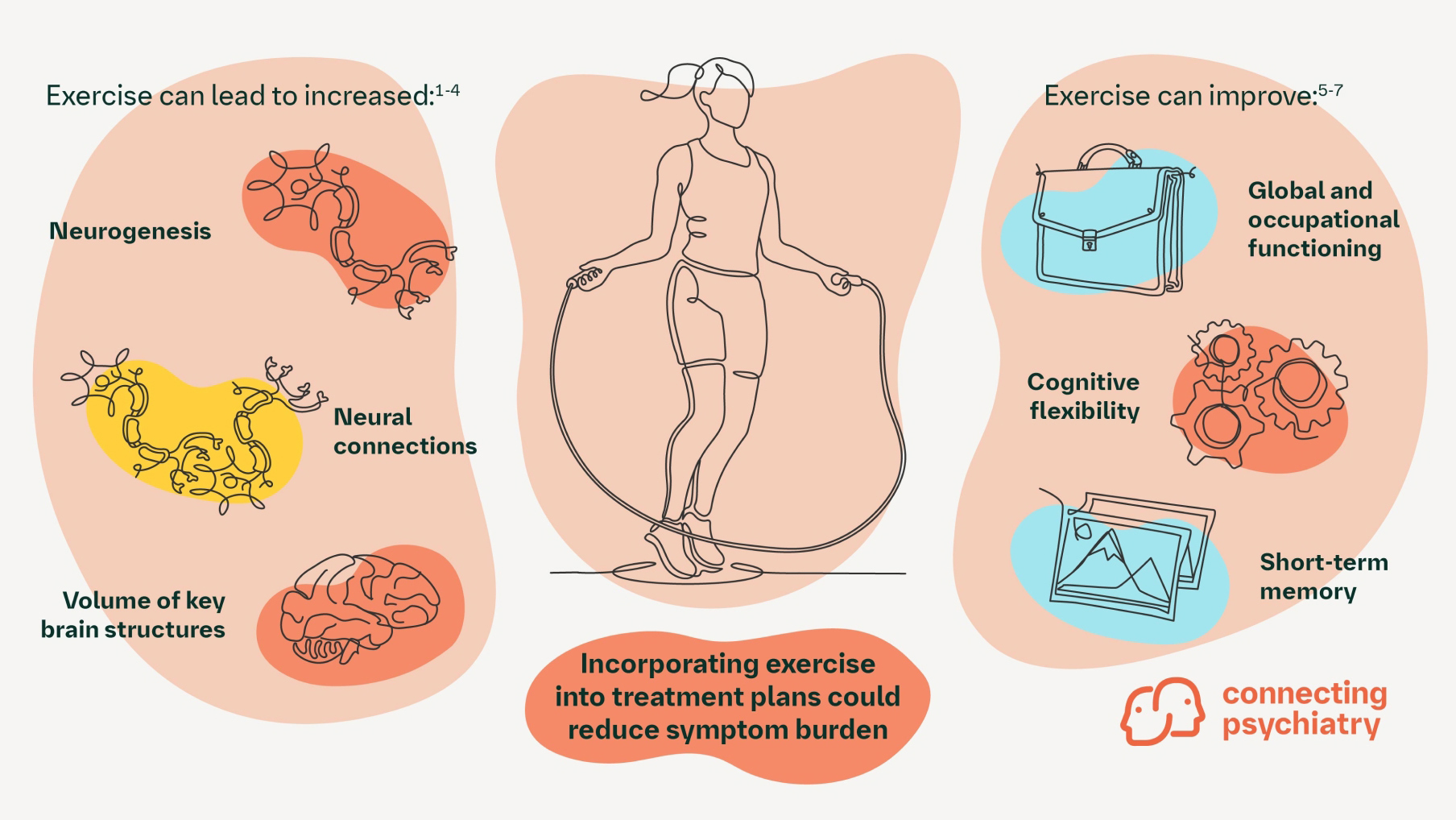
Importantly, recent evidence suggests that exercise can stimulate core physiological changes in the brain, which include increased neurogenesis, plasticity, and neural connections.2 Furthermore, aerobic exercise has been shown to drive volumetric changes in key brain structures commonly affected in mental health conditions, including the prefrontal cortex, subcortex, and mesial temporal structures including the hippocampus.2–4 Thus, exercise regimens may be powerful tools for the treatment of mental health conditions.
The potential impact of exercise on mental health and behavioral outcomes
Individuals with severe mental health conditions such as schizophrenia, bipolar disorder, or major depressive disorder generally spend less time participating in moderate-to-vigorous physical activity, instead spending more time sedentary during waking hours than their healthy counterparts.7 As such, incorporating structured exercise into weekly routines may facilitate improved mental health.7
In fact, routine exercise impacts patient outcomes by reducing symptom burden, improving mental health, and increasing quality of life for individuals with mental health conditions.9,18 Aerobic exercise and strength training have both been shown to improve global and occupational functioning, cognitive flexibility, verbal declarative short-term memory, and global cognition in patients with schizophrenia, as well as lowering the incidence of psychotic episodes.5–7,19 Individuals with major depressive disorder also derive benefit from regular exercise.20 Youths and young adults with major depressive disorder reported moderate benefits of exercise on their overall mental health, including reduced severity and incidence of depressive symptoms, whereas older adults reported a moderate reduction in depressive symptom severity when an exercise regimen was added to their routines.21
Some evidence suggests that the intensity of exercise matters. Rigorous exercise at a high intensity or for too long can be detrimental to mental health.22 Therefore, moderate-intensity exercise may be ideal and ultimately the most beneficial form of exercise for improving overall mental health.
A healthy mind in a healthy body
The numerous health benefits of exercise, including improvements in mental health, have been observed since antiquity, across many cultures around the world.9,23 The principle is well summarized in the Latin mens sana in corpore sano (a healthy mind in a healthy body).24 Growing evidence shows that exercise can reduce symptom burden and improve quality of life for people with mental health conditions.2,15 Taken together, a healthy body indeed leads to a healthy mind, and including exercise as a part of treatment plans for individuals struggling with mental health disorders should be considered as an important facet of patient care.
Further reading
- Maurus I, et al. Exercise as an add-on treatment in individuals with schizophrenia: Results from a large multicenter randomized controlled trial. Psychiatry Res 2023;328:115480.
Results from the ESPRIT C3 randomized controlled trial evaluating the impact of two separate active exercise regimens on symptoms of schizophrenia. - Smith PJ and Merwin RM. The role of exercise in management of mental health disorders: An integrative review. Annu Rev Med 2021;72:45–62.
A review focused on the impacts of physical activity in the management of mental health disorders and symptom burden. - Schuch FB and Vancampfort D. Physical activity, exercise, and mental health disorders: it is time to move on. Trends Psychiatry Psychother 2021;43:177–184.
A review of the evidence that physical activity may have preventative effects for mental health disorders, the role of physical activity in the promotion of overall health, and exercise as a strategy to manage mental health symptoms.
Cite this article as Factor It In: A New Movement for Mental Health. Published May 2024. Accessed [month day, year]. [URL]
-
Liu W, et al. Neural Plast 2017;2017:6871089.
-
Smith PJ and Merwin RM. Annu Rev Med 2021;72:45–62.
-
Falkai P, et al. Eur Arch Psychiatry Clin Neurosci 2022;272:643–677.
-
Takahashi S, et al. Schizophr Res 2020;216:397–407.
-
Landrigan J-F, et al. Psychol Res 2020;84:1167–1183.
-
Maurus I, et al. Dialogues Clin Neurosci 2019;21:261–269.
-
Maurus I, et al. Psychiatry Res 2023;328:115480.
-
Tipton CM. Adv Physiol Educ 2014;38:109–117.
-
Schuch FB and Vancampfort D. Trends Psychiatry Psychother 2021;43:177–184.
-
Centers for Disease Control and Prevention. Benefits of Physical Activity. 2023. Available at: https://www.cdc.gov/physicalactivity/basics/pa-health/. Last accessed: October 2023.
-
Mayo Clinic. Exercise: 7 benefits of regular physical activity. 2023. Available at: https://www.mayoclinic.org/healthy-lifestyle/fitness/in-depth/exercise/art-20048389. Last accessed: October 2023.
-
Vita A, et al. Eur Psychiatry 2022;65:e57.
-
DGPPN e.V. (ed.) S3 Guideline for Schizophrenia. 2019. Available at: https://www.awmf.org/leitlinien/detail/ll/038-009.html. Last accessed: November 2023.
-
American Psychiatric Association. Lifestyle Psychiatry. 2019. Available at: https://www.psychiatry.org/news-room/apa-blogs/lifestyle-psychiatry. Last accessed: October 2023.
-
Caspersen CJ, et al. Public Health Rep 1985;100:127–131.
-
McTeague LM, et al. Am J Psychiatry 2020;177:411–421.
-
Vancampfort D, et al. World Psychiatry 2017;16:308–315.
-
Dauwan M, et al. J Neurol 2021;268:1222–1246.
-
Brokmeier LL, et al. Psychiatry Res 2020;284:112675.
-
Heissel A, et al. Br J Sports Med 2023;57:1049–1057.
-
Ashdown-Franks G, et al. Sports Med 2020;50:151–170.
-
Golshani S, et al. Healthcare (Basel) 2021;9:1289.
-
Tipton CM. Adv Physiol Educ 2014;38:109-117.
-
Kline AS. Juvenal The Satires. Poetry in Translation. 2011.
SC-US-76796
SC-CRP-15096
February 2024

Guideline Digest: Post-traumatic Stress Disorder
Sign up now for new features
The newsletter feature is currently available only to users in the United States
*Required field