Factor It In: Food for Thought
The Factor It In series will illuminate the influences on mental health that arguably deserve greater attention. You will be provided with fresh perspectives through a discussion of the factors that impact the development of serious mental health conditions and a review of the literature on impact on disease course; ultimately, you may use this knowledge to inform discussions with your patient.
In summary
- While there are many factors that contribute to our mental health, one aspect that is often neglected is the influence that gut health can have on mood and mental health
- The microbiota of the gastrointestinal tract interacts with the brain, and its modulation may play a crucial role in the pathophysiology of neuropsychiatric illnesses, including major depressive disorder, anxiety, and other mental health conditions
- Our understanding of the links between the gut microbiome, nutrition, and mental health are evolving; more research is needed to fully understand the mechanisms and interrelationships and their implications for mental health care
How the gut microbiota can modulate neurotransmission
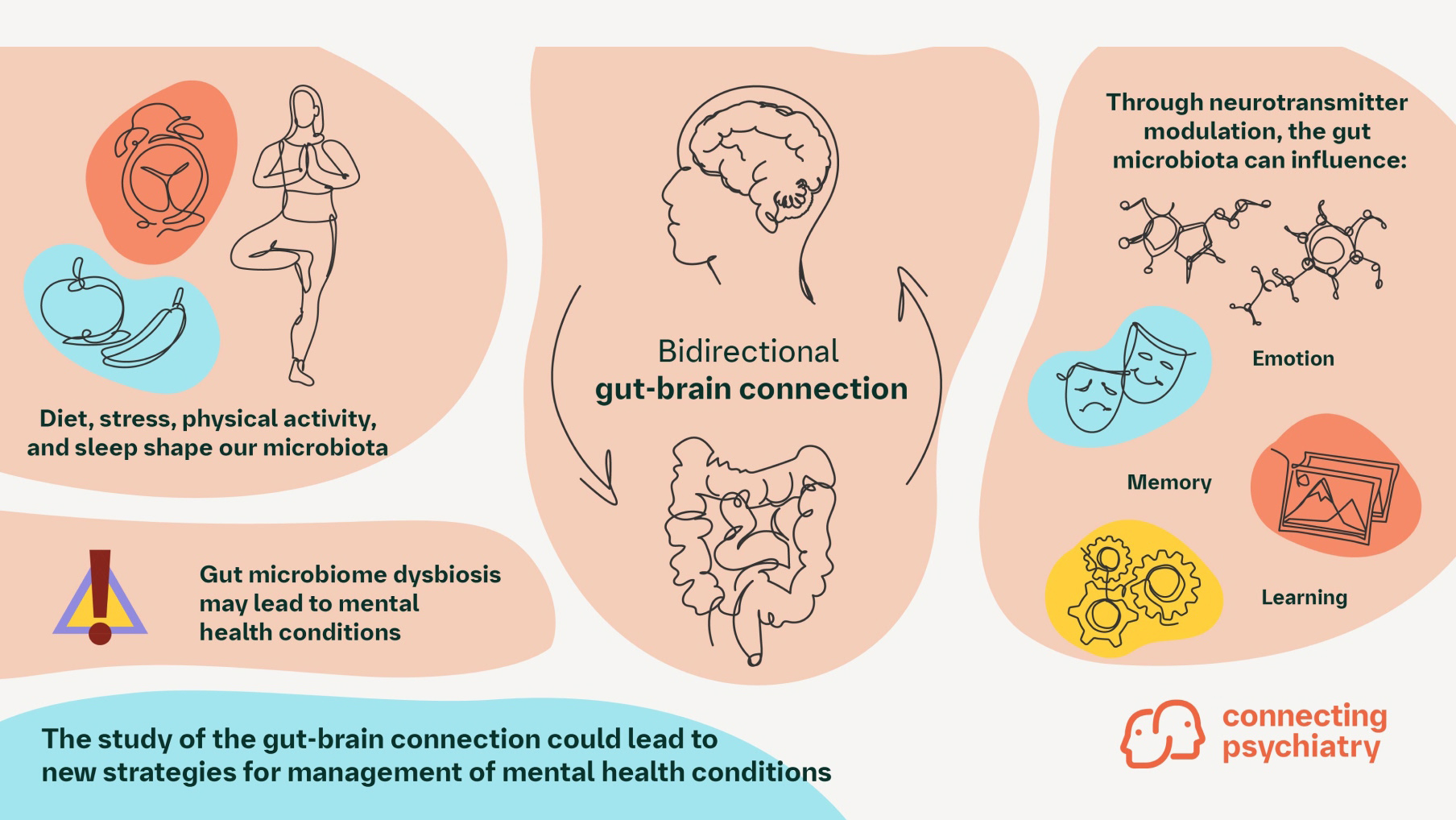
The gut-brain connection refers to the relationship between the gut microbiota and the brain.1 The human gut houses trillions of microbial organisms—including bacteria, viruses, and another class of single-cell organisms called archaea—collectively known as the gut microbiome.2 The gut microbiome interacts with the brain bidirectionally through neural, inflammatory, and hormonal signaling pathways.1,2 Some neuroactive metabolites are produced by the gut microbiota and can impact the concentrations of related neurotransmitters, their precursors, or both in the brain. The neuroactive metabolite production is a mechanism by which the gut can potentially affect emotion, memory, and learning.3 For example, bacterial metabolites such as short chain fatty acids are able to modulate serotonergic neurotransmission.4 Abnormal expression and function of serotonin in the brain has been linked to the pathophysiology of mental health conditions such as depression and anxiety.3 Metabolites of the gut microbiota affect production of various other neurotransmitters, such as gamma-aminobutyric acid, glutamate, serotonin and dopamine, which are important not only for gut function regulation but also for brain function.3–5
Understanding the gut-brain connection in the development of mental health conditions
Disruptions of the gut microbiome, known as dysbiosis, have been correlated with several mental health conditions, including major depressive disorder, anxiety, schizophrenia, and other mental conditions.2,5–7 One of the many causes of dysbiosis is an unhealthy diet consisting of energy-dense and highly processed foods as a well as emulsifiers and artificial sweetners.7,8 An unhealthy diet can compromise the lining of the gut and lead to various imbalances in the gut, such as nutrient deficiencies and leaky gut.7–9 Nutrient deficiencies can have a significant impact on brain and nervous system function and may impact mental health.9–11 Conditions such as leaky gut, which causes gut metabolites to leak into the bloodstream, can trigger immune activation and inflammation.7,8 Continuous immune activation and the inflammation that goes with leaky gut have been implicated in a range of diseases and mental health conditions such as major depressive diorder.6–8 Several studies have reported evidence of diet-related alterations in the gut microbiome and the presence of certain microbial species having an apparent association with several neurological and mental health conditions.5
The food we eat has a direct impact on our gut and mental health
Consuming a balanced diet rich in probiotics and prebiotics can help improve the health of the gut and, in turn, the gut-brain connection.11,12 Probiotics are live microorganisms that can help restore the balance of bacteria in the gut when ingested in adequate amounts.4,7,13 Research on probiotics for mental health shows promise, with some studies suggesting benefits for depression, bipolar disorder, and schizophrenia, but findings remain inconsistent. More evidence is needed to determine their overall effectiveness.4,13 Prebiotics, on the other hand, are non-digestible fibers that serve as a selective food source for the intestinal microbiome, fostering the growth of certain beneficial bacteria and contributing to host health.4,7 While an interesting initial study found improved cognitive function in hospitalized schizophrenia patients using prebiotics, larger studies are required to replicate these findings before definitive conclusions can be drawn.4 Apart from dietary factors, other lifestyle factors such as stress can alter the gut microbiome.8,14 Stress can disrupt the gut microbiome by influencing the complex system of neurotransmitters, inflammatory markers, and neuropeptides present in the gut and brain.14 Stress is associated with alterations in serotonin function in the medial prefrontal cortex and other brain areas involved in the stress response, and altered serotonin function is associated with both depression and posttraumatic stress disorder.14 Understanding the gut-brain connection opens new possibilities for treating mental health conditions.
A young field of study with fascinating potential implications
Although research into the gut-brain connection has accelerated in recent years, it is still in its early stages, and studies vary in terms of study design, study populations, microbiome analyses, and outcomes. Larger sample sizes, longitudinal study designs with longer follow-up periods, consistent methodology, and confounder control are required.15 Despite the limitations of current information, there are several potential approaches with emerging support from preclinical and clinical evidence, such as following an anti-inflammatory, Mediterranean-style diet, or incorporating dietary counseling alongside pharmacological and behavioral multidisciplinary treatment strategies.11 Expanding our knowledge of bacterial species in larger populations with mental health conditions, as well as the influence of medication and dietary habits, could lead to fascinating future developments, such as disease-specific pro/prebiotics.4 Factoring in the gut-brain connection could be a fruitful aspect of a holistic care plan for those with mental health conditions.4
Further reading
- Martins LB, et al. Nutrition-based interventions for mood disorders. Expert Rev Neurother 2021;21:303–315.
The article discusses the current evidence on nutrition-mood interaction and nutrition-based treatments for major depressive disorder and bipolar disorder while reviewing several nutrition-based factors such as dietary patterns and gut microbiome - Mind. Food and mental health. Available at: https://www.mind.org.uk/information-support/tips-for-everyday-living/food-and-mental-health/. Last accessed November 2023.
This site is a useful source and resource center to support discussions with patients about food and mental health.
-
Malan-Muller S, et al. OMICS 2018;22:90–107.
-
Firth J, et al. BMJ 2020;369:m2382.
-
Chen Y, et al. Nutrients 2021;13:2099.
-
Borkent J, et al. Psychol Med 2022;52:1222–1242.
-
Xiong RG, et al. Nutrients 2023;15:3258.
-
Capuco A, et al. Adv Ther 2020;37:1328–1346.
-
Liu L, et al. EBioMedicine 2023;90:104527.
-
Mansour SR, et al. New Microbes New Infect 2021;41:100845.
-
Zielińska M, et al. Nutrients 2023;15:2433.
-
Mörkl S, et al. Neuropsychobiology 2018:1–9.
-
Horn J, et al. Transl Psychiatry 2022;12:164.
-
Fekete M, et al. Nutrients 2024;16:789.
-
Maftei NM, et al. Microorganisms 2024;12:234.
-
Bremner JD, et al. Nutrients 2020;12:2428.
-
Järbrink-Sehgal E & Andreasson A. Curr Opin Neurobiol 2020;62:102–114.
SC-US-76913
SC-CRP-15910
May 2024
Related content
Sign up now for new features
The newsletter feature is currently available only to users in the United States
*Required field


